There has been remarkable progress in digital health innovations and the development and implementation of these has been fast tracked by the coronavirus pandemic. Digital therapeutics, such as mobile applications (apps), wearable devices, telehealth, and similar technologies, facilitate swifter information exchange and streamline medical record access, thereby enhancing efficiency for healthcare providers [1]. In addition, digital therapeutics empower patients to actively manage their health and encourage participation in their treatment plans [2]. In the future, digital therapeutics are anticipated to find widespread application in the management of various chronic diseases. Among the various physiological indicators that can be digitally monitored, the tracking and subsequent management of blood pressure (BP) are particularly well-suited for integration with digital health solutions and has been well researched over the past 20 years [3, 4].
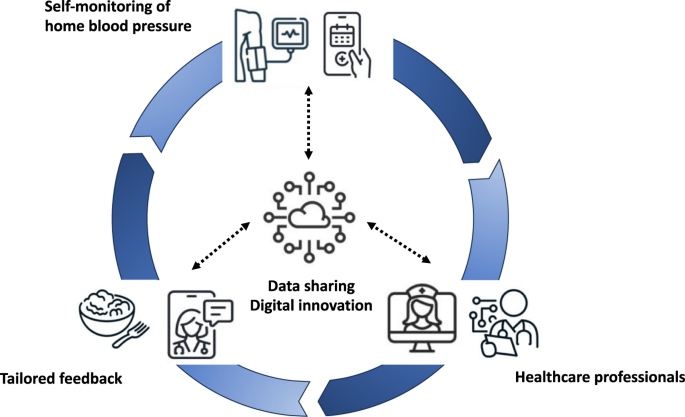
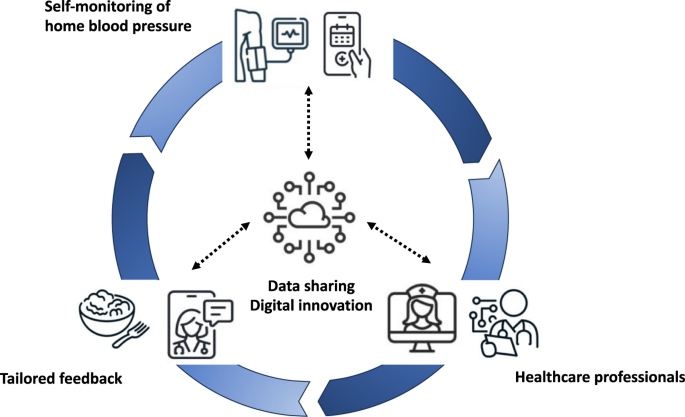
Hypertension guidelines recommend conducting out-of-office BP monitoring for the diagnosis and management of hypertension [5, 6]. Self-monitoring of BP (SMBP) is commonly used for long-term management of hypertension in clinical practice because of its easy availability and low cost [5]. In addition, SMBP with co-interventions, including feedback, education, or lifestyle counseling, by healthcare professionals, was reported to provide significant BP reduction compared to self-monitoring alone [7]. SMBP with the support of healthcare professionals is the cornerstone for the management of hypertension.
Digital therapeutics are gaining traction in medical and healthcare domains and are being utilized for self-management of a range of health conditions, however, there are currently few studies that have focused on evaluating the benefit of digital health interventions in hypertensive patients, and their findings are varied. Meng et al. demonstrated that the home BP telemonitoring plus support (including patient education and physician remote hypertension management) group showed greater reductions of ambulatory BPs (including 24-hr, daytime and nighttime BPs) and higher rates of hypertension control than the usual care group (home BP monitoring alone) after 12 weeks of follow-up [8]. On the other hand, the Telemonitoring and Self-Management of Hypertension Trial (TASMINH4) showed that there was no significant difference between the group of self-monitoring with telemonitoring and that of self-monitoring alone in the reductions of BP level after 6 months and 12 months of follow-up [9].
In a Japanese population of untreated patients with essential hypertension, the HERB Digital Hypertension 1 (HERB-DH1) pivotal trial highlighted the effects of a digital intervention for non-pharmacological lifestyle modification to reduce BP levels [10]. Patients were randomly assigned to the digital therapeutics group or the control group. Patients allocated to the digital therapeutics group managed their home BP using the HERB application and implemented a personalized program of lifestyle modifications based on the data. On the other hand, patients allocated to control group were provided standard lifestyle modification alone. After 12 weeks of follow-up, the digital therapeutics group showed significant reductions from baseline in 24-h ambulatory, morning home, and office systolic BP compared with the control group. Furthermore, these trials demonstrated that digital interventions may offer a cost-effective alternative to conventional treatments in lowering BP levels [11]. Based on these trial results, hypertension application-based treatment has been covered by insurance for the first time in September 2022 in Japan. In the future, as this approach becomes widely integrated into routine clinical practice, it is anticipated that personalized and continuous patient support will be facilitated. Additionally, it is expected to lead to a reduction in healthcare provider consultation time and serve as a strategy to overcome clinical inertia by offering advice on the appropriate intensification of treatment [3]. In the future, it is expected to elucidate the impact of mobile health (mHealth) on hypertension management in real-world clinical settings.
The present study conducted by Kishi et al. [12]. demonstrated the potential benefits of digital intervention, showing an improvement in hypertension control rates and a reduction in home BP levels among patients with essential hypertension after 6-month follow-up. Examining the results of this study, some pieces of relevant information need to be mentioned. First, patients in this study simply monitored their daily home BP levels, medication adherence, and lifestyle habits using their app, without education or lifestyle modification programs. Lifestyle modification and non-pharmacological treatment are important approaches in the management of hypertension [5, 6]. Second, the patients enrolled in this study were middle-aged, able to use smartphones, and were considered to be a relatively healthy population. When considering the use of apps in daily clinical practice, easy utilization by a wide range of age groups, including the older population, and patients with multimorbidity is desirable and would need further testing in this case. Additionally, establishing a support system for digital literacy among older population may be needed. Third, HMS needed physicians to check patients’ home BP data before they visited the clinic. In everyday clinical practice, a system that allows for easy and convenient access to daily patient data without causing undue burden is desired. The utilization of an alert system capable of automatically notifying healthcare professionals about home BP values outside the therapeutic target range would be a beneficial option, ideally through integration with the electronic health recoed [13]. In addition, to enhance the generalizability of digital intervention using mobile apps, it is imperative to improve their interoperability with existing medical record systems [3]. Fourth, although physicians monitored patients’ home BP levels, medication adherence, and lifestyle habits before a scheduled clinic visit on the website connected to HMS, some patients may feel burdened by the prospect of physicians monitoring such indicators. Sensitivity towards such patients and ensuring privacy are crucial. It is also important to ensure supportive relationships between clinical teams and patients. Moreover, for the widespread adoption of digital therapeutics, ensuring data security is essential.
Currently, a large number of mHealth apps are available worldwide. However, there is a lack of evidence regarding the long-term benefits they confer in terms of BP management and, furthermore, their contribution to cardiovascular disease (CVD) event prevention. Krzowski et al. recently showed that mHealth interventions for patients after myocardial infarction may improve their CVD prognosis [14]. After 6-month follow-up, the intervention group who received digital support using a mobile app showed significantly lower N-terminal pro-brain natriuretic peptide levels, better knowledge regarding CVD risk factors, and tended to show lower rate of rehospitalization and/or urgent outpatient visit, compared to the control group. Further research is needed to provide evidence of the promising potential of mHealth in enhancing the long-term prognosis of CVD.
Management of chronic diseases is a complex process shaped by three key stakeholders: the clinician, the patient, and the health care system [15]. It is expected that medical innovations in hypertension management will further accelerate in the future, leading to the development of effective and user-friendly apps. Healthcare professionals should carefully and fully discuss how these state-of-the-art devices can be implemented into the existing healthcare delivery systems. In addition, in order to offer hypertensive patients care that is accessible to all, continuous, and tailored to their specific needs, a multidisciplinary team-based approach is required (Fig. 1). Kishi et al. [12]. provided useful information for healthcare professionals, demonstrating the enormous potential of mobile app interventions for the management of hypertension. To establish more robust evidence regarding the effectiveness of mHealth apps, further larger-scale controlled studies and research demonstrating utility in real-world clinical settings are necessary.
TF received funding from the SENSHIN Medical Research Foundation. RM and KT have received research funding from the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research Oxford and the Thames Valley (ARC-OxTV), and from an NIHR programme for Applied Health Research (Ref: NIHR203283). RM is an NIHR Senior Investigator. The views expressed in this publication are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health and Social Care.